Long Case General medicine Final practical Exam
This is a online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patients problems through series of inputs from available global community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs .This E log book also reflects my patient centered online learning portfolio and your valuable inputs in comment box is welcome.
CHIEF COMPLAINTS:
38 year old female Came to OPD with an Chief complient of : Poor stream of urine since 1 month.
Dysuria (painful urination) since 18 days
Burning micturition since 13 days
Pain in lower abdomen since 13 days
History of Present illness :
Patient was apparently asymptomatic 1 month back , then she developed poor stream of urine
she developed pain during micturition since 18 days.
Pain in lower abdomen Spasmodic type of pain
non radiating with no aggrevating and relieving factors
Burning micturition since 13 days.
Patient had H/O urinary retention , poor stream of urine and burning micturition
No H/O fever, vomitings,nausea,increased frequency,loose stools .
MENSTRUAL HISTORY
Cycle - 5/30 days and regular
She had history of 2 abortions
1st abortion at age of 19Years old
2nd abortion at age of 20Years old
PAST HISTORY:
Not a k/c/o DM, HTN , TB ,epilepsy, asthma,CAD,CVD.
she was diagnosed with urethral stricture 1 year ago and underwent dilitation 1 year ago
PERSONAL HISTORY:
Diet - mixed
Appetite - Normal
Sleep - adequate
Bowel - regular
Bladder - burning micturition, dysuria
Addictions - She has habit of chewing PAN since 7years
FAMILY HISTORY:
No significant family history
GENERAL EXAMINATION:
Patient is concious coherent and cooperative and well oriented to time place and person
Pallor is present .
No icterus, cyanosis, clubbing, lymphadenopathy , pedal edema
Vitals -
Temp -98.6F
PR - 74bpm
BP - 120/70 mmhg
RR - 18cpm
SYSTEMIC EXAMINATION :
ABDOMEN :
Inspection :
All quadrants are moving equally with respiration
No sinuses , engorged veins, visible pulsations .
Distension of lower abdomen
Palpation :
Abdomen is Soft
Tenderness present on right hypogastric region
Percussion :Tympanic note heard over the abdomen
Auscultation:
Bowel sounds are heard.
CARDIOVASCULAR SYSTEM
Inspection:
Shape of chest is elliptical.
Palpation: Apex beat - felt at left 5th intercostal space. No thrills and parasternal heaves
Auscultation :
S1 and S2 heard.
RESPIRATORY SYSTEM:
On Inspection:
Shape- elliptical
B/L symmetrical
Both sides moving equally with respiration
On Palpation:
Trachea - central
Expansion of chest is symmetrical.
Vocal fremitus - normal
Percussion: resonant bilaterally
Auscultation:
bilateral air entry present.
vesicular breath sounds heard.
CENTRAL NERVOUS SYSTEM:
Conscious,coherent and cooperative
Speech- normal
Sensory System - Normal
Motor system - Normal
ORAL EXAMINATION :
Gingival recession is seen
Spacings between the tooth (Malocclusion)
Loss of taste sensation (Atrophy of tongue/papilla)
Xerostomia (decreased saliva production)
Looks like hypocalcification of ENAMEL
Calculus++
Stains++
Pateint has poor oral hygiene
Clinical Pictures :
INVESTIGATIONS
HEMOGRAM
COMPLETE URINE EXAMINATION
BLOOD UREA
USG
ECG
XRAY
PROVISIONAL DIAGNOSIS:
RECURRENT STRICTURE URETHRA WITH IDA.
TREATMENT :
Tab Norflox 400
Tab Ascofer-XT
UROLOGY opinion was taken and Adviced for FOLEYS CATHETERIZATION
In view of sever pain during CATHETERIZATION procedure was done
Retention volume=1500ml urine after catheter was placed
Urologist Adviced need for "URETHROPLASTY"
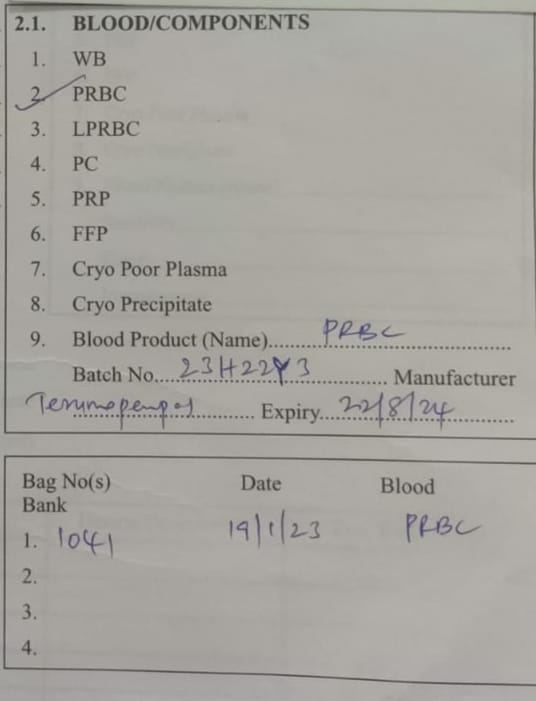
As patient was Anemic - Need for correction of HEMOGLOBIN for prior surgery.





















Comments
Post a Comment